

Furthermore, the characteristics of idiopathic FBS have not been thoroughly investigated.
As such, it poses a diagnostic challenge for even the most experienced pain clinicians. In rare cases, FBS may be idiopathic therefore, it may be overlooked or easily misdiagnosed during the evaluation of facial pain. Recent studies have documented parotid pain compatible with FBS in patients with diabetes. However, diabetic neuropathy is another potential cause of FBS. FBS may rarely occur in patients without a history of surgery of the upper cervical region or evidence of an underlying tumor. The reports suggest that FBS is associated with tumors, namely, malignant tumors arising from the parapharyngeal space, parotid gland, or submandibular gland and benign tumors of the temporal bone. įBS in the absence of prior surgical intervention is rare therefore, it has mainly been described only in case reports. Collectively, these factors suggest that the loss of sympathetic innervation to the parotid gland and consequent denervation hypersensitivity of the parotid myoepithelial cells cause FBS pain. The strongest independent factors for FBS are parapharyngeal space dissection, resection of only the deep lobe of the parotid gland, and sympathetic chain sacrifice. FBS mainly occurs after upper neck surgery therefore, most studies have focused on the association between FBS development and operative procedures. The etiology and pathogenesis of FBS remain to be elucidated. However, owing to the limited number of cases that have addressed the management of FBS, there is no established therapy for this condition. Potential treatments for relieving FBS pain include dietary modifications, pharmacological interventions, and botulinum toxin injection. Patients may avoid eating because of the severity of FBS pain. Introductionįirst bite syndrome (FBS) is a relatively rare clinical condition in which the first bite of each meal causes severe pain or cramping that gradually subsides with subsequent mastication. Thus, it is necessary to consider idiopathic FBS during the evaluation of facial pain triggered at the beginning of a meal. Our findings indicate that the characteristics of idiopathic FBS in patients without diabetes are largely consistent with those previously reported in postoperative FBS, supporting the notion that idiopathic FBS is a subtype of FBS. Two patients presented with ipsilateral idiopathic Horner’s syndrome. Two patients had tenderness on mild pressure over the affected parotid region. Idiopathic FBS was bilateral in two patients. The median degree of pain intensity and interference with eating due to pain was 9 (range: 3–10) and 9 (range: 5–10) on a numerical rating scale of 0–10, respectively. Addition of an acidic solution to the ipsilateral posterior third of the tongue evoked parotid pain. All patients immediately experienced parotid pain upon tasting food without chewing. Four of the five patients were female, and the overall median age was 52 years (range: 13–61). We retrospectively analyzed the clinical data of five patients without diabetes who were diagnosed with idiopathic FBS in our department between January 2010 and December 2016. We aimed to identify the clinical and pain-related characteristics of idiopathic FBS in patients without diabetes. Idiopathic FBS in patients without diabetes may be overlooked or misdiagnosed because the condition has been described only in a few case reports.
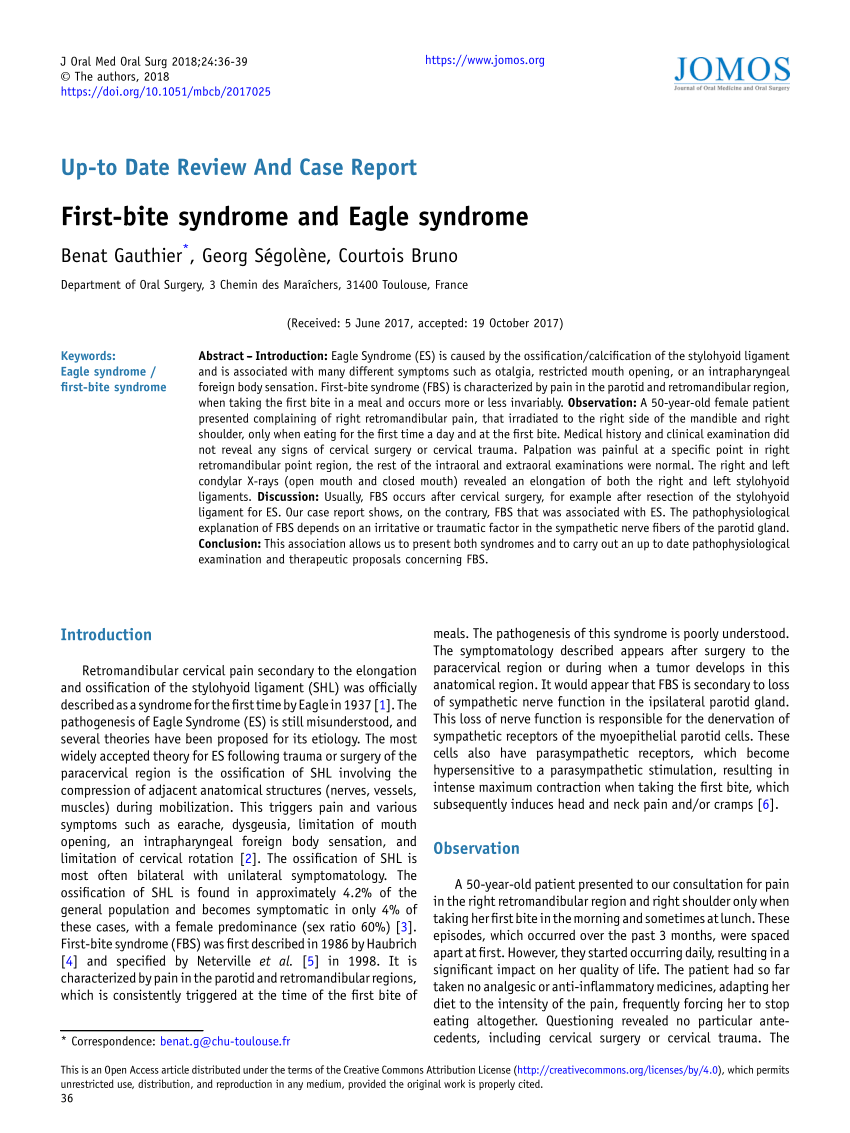
Idiopathic FBS may be categorized into two subtypes: that in patients with diabetes and that in patients without diabetes. Idiopathic FBS rarely presents in patients without a history of surgery or evidence of an underlying tumor. Etiologies of FBS include prior surgery of the upper cervical region and, rarely, head and neck tumors. First bite syndrome (FBS) is a condition in which the first bite of each meal causes parotid pain.


 0 kommentar(er)
0 kommentar(er)
